The Finding
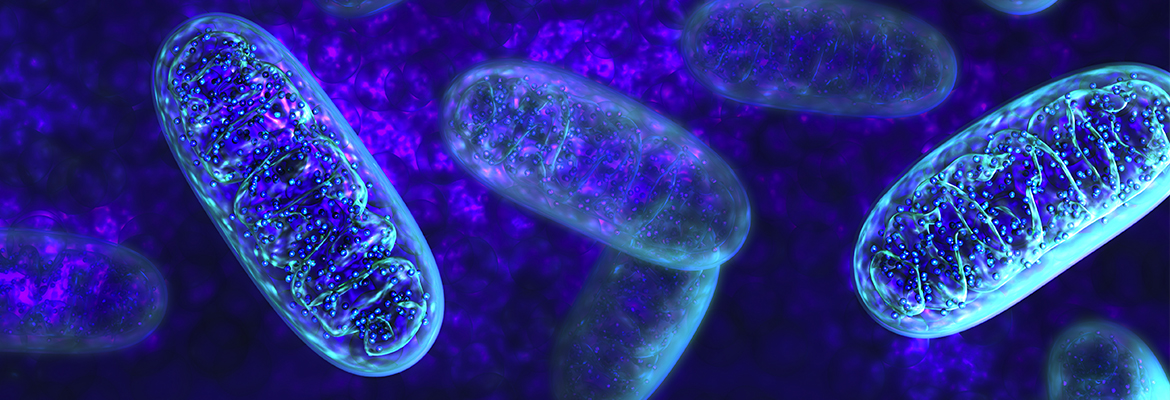
An international research team led by a Children’s Hospital of Philadelphia geneticist classified a new craniofacial disorder tied to disruptions in our cell’s tiny protein transport systems. The researchers identified the genetic disorder, ARCN1-related syndrome, in three children and an adult who share similarities in clinically recognizable facial differences, small heads and limbs, and mild developmental delays. As the condition’s name suggests, the four patients also share mutations in archain 1 (ARCN1) — a gene that encodes proteins in one of the body’s delivery systems for transporting, or “trafficking,” proteins between structures inside our cells: the COPI system. Previous research has linked the COPI system to neuronal functions, so the ARCN1 mutations may also affect brain development.
Why it matters
Families of children with rare disorders often experience stress as they embark on a series of tests and unsuccessful treatments known as “diagnostic odysseys” with no clear explanation for their complex condition. Putting a definitive name to a rare set of symptoms — and learning that other individuals share the same diagnosis — offers relief for patients while also bringing researchers one step closer to developing effective treatments.
Who conducted the study
Kosuke Izumi, MD, PhD, attending physician in the Roberts Individualized Medical Genetics Center and the Division of Human Genetics at CHOP, led the study with colleagues from the University of Tokyo, Nagano Children’s Hospital, KK Women and Children’s Hospital, Shinshu University Graduate School of Medicine, Hopital Robert Debre, Centre Hospitalier Universitaire et Université de Liège, St Thomas’ Hospital, Genome Institute of Singapore, and SingHealth Duke-NUS Medical School.
How they did it
The researchers sequenced the exomes (the protein-coding portions of DNA) of the four patients and found loss-of-function mutations in the ARCN1 gene, which plays a role in the COPI system. COPI governs the transport of proteins between the cell’s endoplasmic reticulum (ER) and the Golgi apparatus so that when a mutation in ARCN1 disrupts the cell’s normal protein trafficking route, protein accumulates in the ER to cause a stress response that kills cells. ER stress can also impair the secretion of collagen — an important part of the connective tissue within bone and cartilage.
Quick thoughts
“This genetic syndrome represents a novel class of disorders,” Dr. Izumi said. “We have reported only the second known disease associated with the COPI protein complex, one of the three key intracellular protein transport systems.”
What’s next
Finding the cause of ACRN1-related syndrome is just the first step: The researchers will continue to identify more children and adults with similar symptoms, as well as conduct further studies to investigate COPI transport’s role in bone formation. “In order to provide better care for children with ARCN1-related syndrome, we still need to understand the full clinical spectrum of this disorder,” Dr. Izumi stated. “At the same time, we need to better understand the disease mechanism in order to discover therapies.”
Where the study was published
The study was published in the American Journal of Human Genetics.
Who helped fund the study
Grants from the Japanese governmental agency MEXT, Core Research for Evolutional Science and Technology, the Japan Agency for Medical Research and Development, the Singapore Ministry of Health, and the French Ministry of Health supported this research.
Where to learn more
You can learn more about this research in the press release and read the study abstract online. To find out about genetics research at CHOP, see the Roberts Individualized Medical Genetics Center and the division of Human Genetics.